Impaired Energy Production May Explain Why the Brain Is Susceptible to Age-Related Diseases
(Originally published by The Salk Institute)
May 29, 2018
Defective energy production in old neurons might explain why our brains are so prone to age-related diseases. Salk researchers used a new method to discover that cells from older individuals had impaired mitochondria—the power stations of cells—and reduced energy production. A better understanding of the effects of aging on mitochondria could reveal more about the link between mitochondrial dysfunction and age-related brain diseases, such as Alzheimer’s and Parkinson’s. The work appeared in Cell Reports on May 29, 2018.
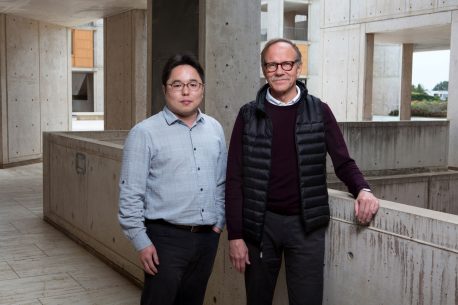
“Most other methods use chemical stresses on cells to simulate aging,” says senior author Rusty Gage, a professor in Salk’s Laboratory of Genetics and the Vi and John Adler Chair for Research on Age-Related Neurodegenerative Disease, and co-director of the Kavli Institute of Brain and Mind at the University of California, San Diego. “Our system has the advantage of showing what happens to mitochondria that age naturally, within the human body.”
Mitochondria, small structures found within cells, are responsible for converting our food into chemical energy our cells can use. Defects in mitochondrial genes can cause disease, but researchers also know that mitochondria become less efficient with aging and can drive age-related disorders.
Previously, the Gage lab developed a method to directly convert skin cells into neurons (called induced neurons, or iNs). Most methods to create neurons from patient cells rely on an intermediary stem cell step (creating what are called induced pluripotent stem cells), which resets cellular markers of aging. But the Gage lab’s iNs retained signs of aging, including changes to gene activity and the cells’ nuclei, the team reported in 2015.

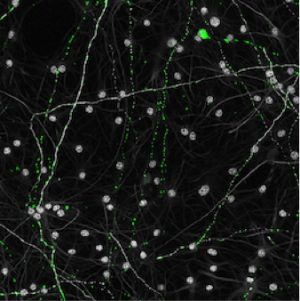
In the new work, the researchers asked whether mitochondria in the cells also retained hallmarks of aging during the iN conversion process. Using skin cells collected from humans ranging in age from 0 to 89 years old, the team created iNs from each donor and then used a variety of methods to study the mitochondria of each set of cells.
Mitochondria in the skin cells isolated from each person showed few age-related changes. However, once the cells were directly converted to neurons, mitochondria from older donors were significantly different. Mitochondrial genes related to energy generation were turned off and the mitochondria were less dense, more fragmented and generated less energy.
“Pretty much every area we looked at—functional, genetic, and morphological—had defects,” says Jerome Mertens, a Salk staff scientist and co–corresponding author of the new paper.
The researchers hypothesized that the reason the mitochondria of iNs were more impacted by aging than the mitochondria of skin cells was that neurons rely more heavily on mitochondria for their energy needs. “If you have an old car with a bad engine that sits in your garage every day, it doesn’t matter,” Mertens says. “But if you’re commuting with that car, the engine becomes a big problem.”
The finding shows how aging can impact organs differently throughout the body.
The researchers next want to begin to apply their method to study age-related diseases, including Alzheimer’s and Parkinson’s. In the past, mitochondrial defects have been implicated in these diseases. By collecting skin cells from patients and creating iNs, the team can look at how neuronal mitochondria from patients with those diseases are different from neuronal mitochondria from unaffected older individuals.
“There is no other in vitro human neuronal model to study aging,” says Yongsung Kim, a research associate and first author of the paper. “So the big takeaway from our paper is that we developed a tool that enables us to study neurological aging and age-related diseases.”
Other researchers on the study were Xinde Zheng, Zoya Ansari, Mark Bunnell, Joseph Herdy, Larissa Traxler, Hyungjun Lee, Apua Paquola, Chrysanthi Blithikioti, Manching Ku, Andres Paucar, Baptiste Jaeger, Son Pham, Leah Boyer, Benjamin Campbell and Tony Hunter of the Salk Institute; Johannes Schlachetzki and Jürgen Winkler of Friedrich-Alexander University Erlangen-Nurnberg; Frank Edenhofer of Leopold-Franzens-University Innsbruck; and Christopher Glass of the University of California San Diego.
The work and the researchers involved were supported by grants from the Paul G. Allen Family Foundation, the National Institute on Aging, the Austrian Science Fund, the Shiley-Marcos Alzheimer’s Disease Research Center, the JPB Foundation, the Glenn Foundation Center for Aging Research, the American Federation for Aging Research, the Leona M. and Harry B. Helmsley Charitable Trust, Annette Merle-Smith and the Mathers Foundation, the California Institute for Regenerative Medicine, the G. Harold and Leila Y. Mathers Charitable Foundation, a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation, and the National Cancer Institute.