Neural Patterns
by Sally Johnson
Mathematical modeling is advancing our understanding of epilepsy, and enabling researchers to get more use out of data

The Author
The Researcher
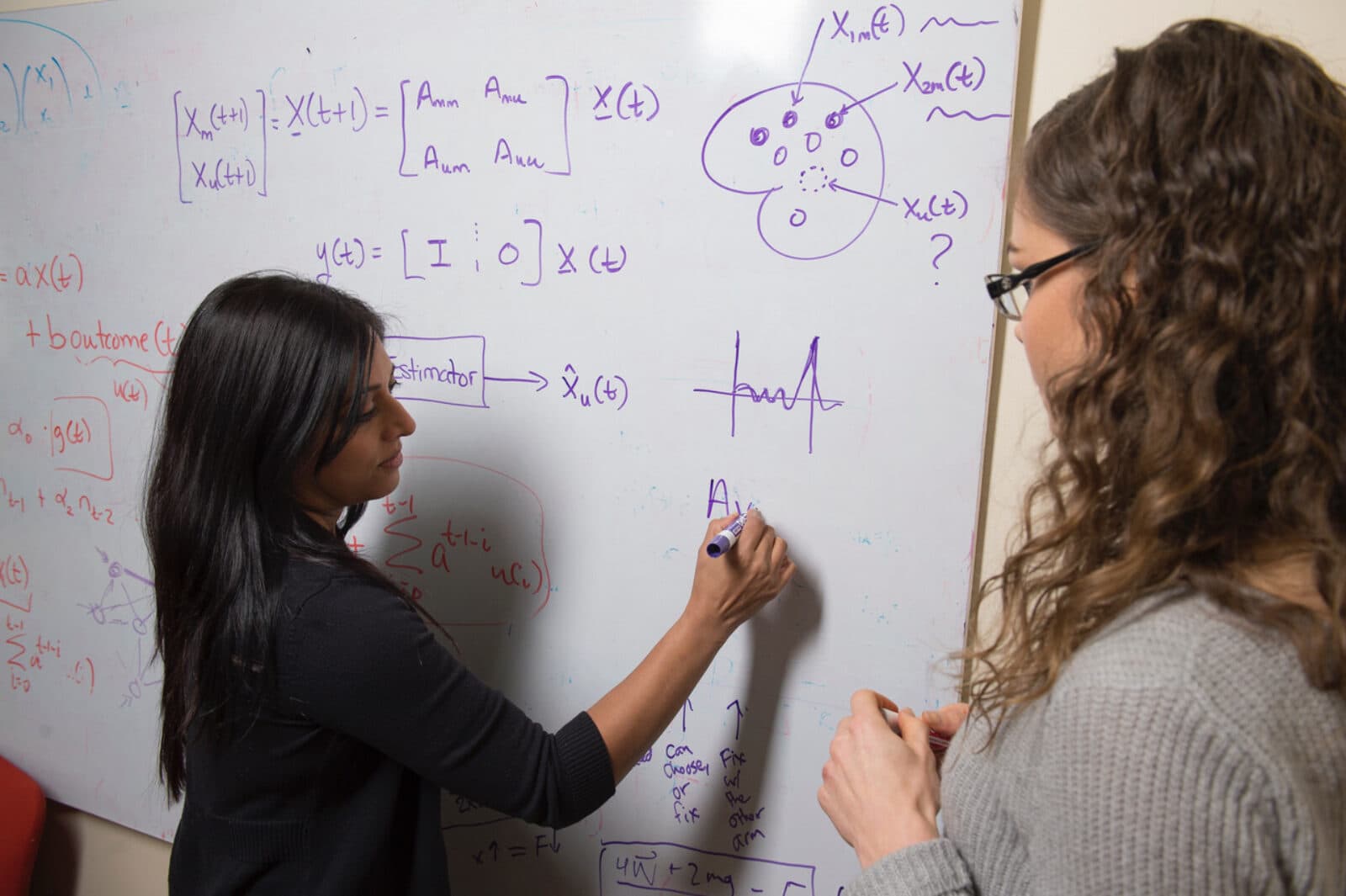
In Sridevi V. Sarma’s lab at Johns Hopkins University, computational neuroscience tools are revealing how neural patterns work within the brains of patients with epilepsy and chronic pain.
Sarma is an associate professor of biomedical engineering in the Institute for Computational Medicine, as well as a faculty member of the Kavli Neuroscience Discovery Institute, and works closely with clinicians to help them better diagnose and treat patients with epilepsy and chronic pain.
“I’m an electrical engineer by training, and started out studying control theory and dynamical systems,” she explains. “Most people with this training go work for Boeing or Ford where they design controllers for airplanes or cars. But I was interested in neuroscience and minored in it while working on my PhD. For one of the courses, Systems Neuroscience, we studied the various systems of the brain—visual, auditory, motor systems, and so forth. And for motor systems, we studied disorders such as Parkinson’s disease. At that time, my aunt was diagnosed at just 28 years old—a very rare case. Most people are diagnosed in their 60s.”
For the next 10 years, Sarma embarked on a journey to explore which neural patterns are affected and how they change in Parkinson’s disease, starting with a postdoctoral fellowship as well as the first seven years of her career at Hopkins.
More recently, Sarma’s focus has turned to neural patterns in epilepsy. Drug-resistant patients whose seizures aren’t controlled by any combination of medications must turn to surgery or stimulation for treatment. “The surgical success rate averages 50%—that’s where we are in 2021,” she points out.
To plan a surgery, clinicians first try to find where seizures start in the brain so they can go on to surgically remove that tissue in the hopes of preventing future seizures.
When clinicians search for seizure onset zones, they often implant electrodes inside the patient’s brain. While the patient recovers, they sit in a monitoring room for several weeks. Clinical teams wait to see if they have seizures so they can look at the electroencephalograms (EEGs) and data captured inside the brain.
“These are highly invasive recordings in humans,” says Sarma. “And we noticed that while patients recover from the implantation in the hospital, they’re bored. So we got funding from the National Science Foundation to run some behavioral tests. One was decision-making in a gambling task—basically a game of war with a deck of cards.”
Ten patients gambled with a computer, while recordings from more than 80 structures inside their brains were simultaneously captured at millisecond resolution—essentially at the source. “It was the first time we know of that these types of recordings were made in humans while gambling,” Sarma notes.
They discovered some gamblers weren’t betting based on odds, and Sarma’s group wondered if there was an internal bias going on, or gut feelings that were unobservable.
So they brought in dynamical systems models to estimate latent states. “The bias of how you feel is not something you can measure, so you need to estimate it from measured data,” Sarma explains. “Mathematical models allow us to do this—they’re simple and tractable, and we can analyze them.”
When they estimated this internal bias, essentially how the gamblers felt, they found this risk-taking bias is caused by high-frequency activity on the right side of your brain. “If you were dealt a card and didn’t have a high chance of winning, you’d be more likely to take a risk if you have this high-frequency rhythm in your right hemisphere,” Sarma says. “If it’s in the left hemisphere, you’re less likely to take a risk. It’s like having the devil sitting on your right shoulder and an angel sitting on your left—through patterns within your brain.”
In other epilepsy work, Sarma’s lab set out to search for a biomarker of the seizure onset zone. “During the past seven years, we developed an intracranial EEG biomarker. We took recordings clinicians are already getting from a patient, specifically capturing seizure events, and built a software tool to compute the biomarker, which is the neural fragility.”
They believe the most fragile areas of the brain are behind seizures. “Fragility is a measure of how a particular region in the brain is connected to its neighbors, so if it’s connected in a faulty way it can trigger seizures,” Sarma says.
And her lab found a way to quantify this abnormal activity. They created software to compute fragility over all regions of the brain that are being sensed, which produces a simple map that can be read right on the brain. “Red areas highlight where physicians should treat,” Sarma says. “We commercialized our software for clinical use, and it was FDA cleared in December 2020.”
Now, Sarma’s lab is exploring a similar way to capture biomarkers while patients are simply resting in their beds—rather than experiencing seizures. “Recordings captured while patients are at rest are completely ignored,” she says. “This is terabytes of data clinicians don’t even look at because why look at signals while patients are at rest? It just looks like white noise, static.”
One of her PhD students, Kristin Gunnarsdottir, has a hypothesis: Since seizures don’t occur all the time, other areas of the brain must be constantly inhibiting the seizure onset zone.
Biological evidence suggests this is happening, so they are using “white noise” to find the groups of nodes stopping seizures by looking at areas they point to and influence. “She’s showing she can identify where seizures start with almost the same level of accuracy as when clinicians actually look at a seizure,” says Sarma.
If they can demonstrate its reliability, “clinicians won’t need to wait weeks for patients to have a few seizures to be confident in their diagnosis,” she adds. “In an ideal world, maybe they won’t even need to see a seizure. They can put the implants in for a couple of hours, take them out, and go to surgery. It would be a game-changer in terms of the treatment paradigm.”